Blog
Spatial transcriptomics uncovers new treatment pathways for triple-negative breast cancer
In a recent study published in the journal researchers are analyzing tumor architecture, cell composition, and the microenvironment in patients with triple-negative breast cancer (TNBC) using spatial transcriptomics and histomorphological analysis. A total of nine TNBC spatial archetypes were identified and associated with disease outcomes and actionable characteristics, as well as a tertiary lymphatic gene signature that predicts immunotherapy answer.
Characteristics of TNBC
Approximately 15–20% of all breast cancer (BC) patients suffer from TNBC, a malignancy with a poor prognosis due to its heterogeneity and lack of effective treatment options. Multi-omics analyzes of bulk tumors have identified five molecular subtypes in TNBC, including basal-like (BL), immunomodulatory (IM), luminal androgen receptor (LAR), mesenchymal (M), and mesenchymal stem-like (MSL).
TNBC subtypes differ in their genomic, transcriptomic and tumor microenvironment profiles, with different prognoses and therapeutic implications. For example, due to high expression of immune genes, the IM subtype is associated with better outcomes and potential response to immunotherapy. In comparison, the LAR subtype, which is characterized by androgen receptor expression and frequent phosphatidyl-nositol 3-kinase (PIK3CA) mutations, is associated with worse treatment outcomes.
The tumor microenvironment, including tumor-infiltrating lymphocytes (TILs) and lymphoid aggregates, is increasingly recognized as a key factor in prognosis and response to treatment. However, traditional ribonucleic acid (RNA) sequencing of bulk tumors fails to capture intratumoral heterogeneity, clonal interactions, and the spatial organization of the tumor microenvironment.
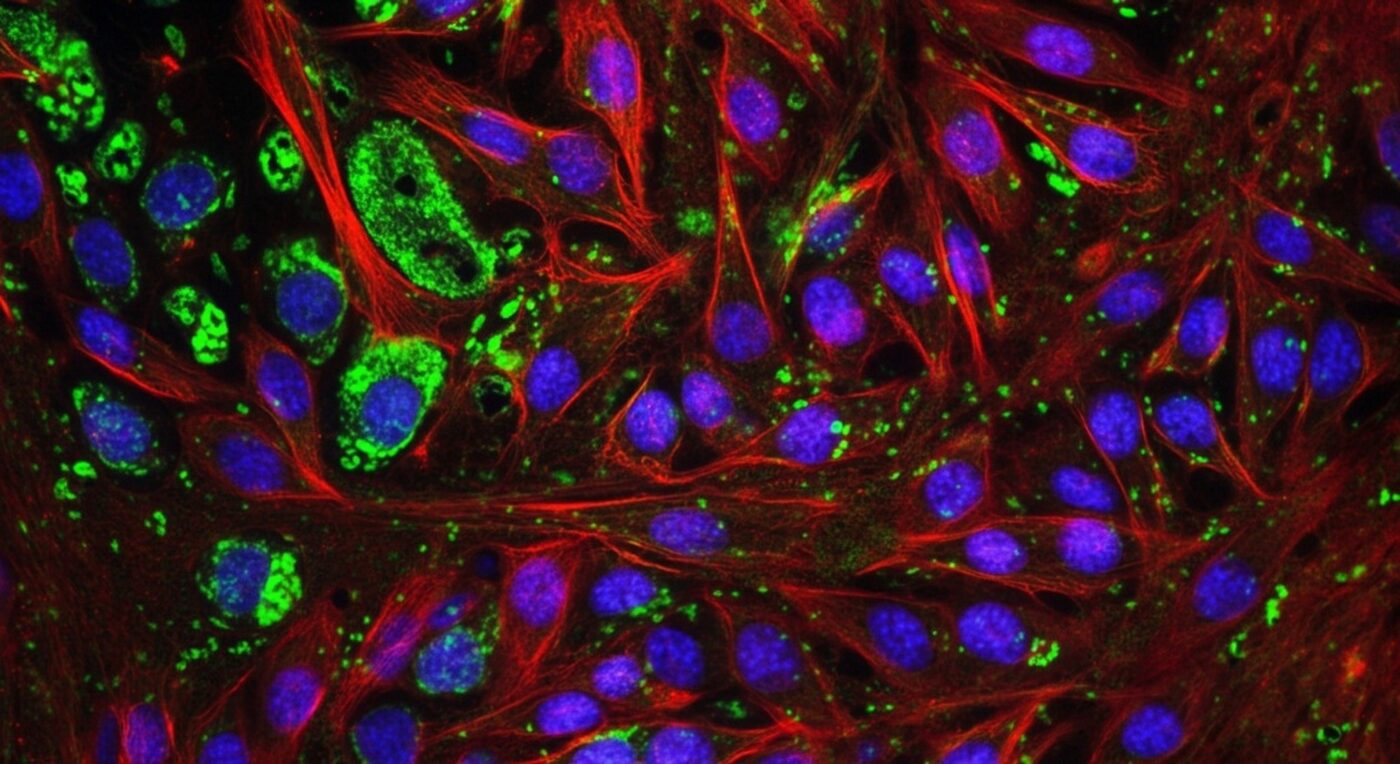
Spatial transcriptomics (ST) has emerged as a powerful tool for the spatial processing of transcriptomic data in cancer tissues and has provided unprecedented insight into tumor heterogeneity and microenvironment interactions. Although ST is still in the early stages of BC research, it is a promising tool that can improve our understanding of the complexities of TNBC and guide the development of targeted therapies.
About the study
In the present study, investigators use ST on TNBC tumors to analyze intratumor heterogeneity, tumor stromal interactions, and immunological features to identify clinically relevant spatial archetypes and a predictable tertiary lymphoid structure (TLS) gene signature.
The current study included a total of 94 patients with early-stage TNBC treated between 2000 and 2016, from whom 96 frozen tumor samples were obtained for ST analysis. Tumor sections were histologically annotated and classified according to tumor immune microenvironment (TIME) immunophenotypes.
Tumor samples were also analyzed for tumor stromal composition, tertiary lymphoid structures, and morphological features. Massive RNA sequencing was performed to verify transcriptomics.
External validation data sets from the METABRIC, SCAN-B, I-SPY2, and non-BC immunotherapy cohorts were used for intercohort analyses. Morphological and transcriptomic data were integrated to identify critical immune and tumor-stroma interactions, spatial patterns, and clinically relevant biomarkers. Essential TNBC-related genes were selected for detailed study based on their biological and therapeutic importance.
Research results
High-quality sequencing data was obtained for 281 subarrays from 92 patients, for a total of 270,310 spatial transcriptomic spots. Molecular subtypes have been associated with distinct patterns.
Specifically, the IM, BL, and M subtypes were enriched in tumor content, whereas the LAR and MSL subtypes had more stroma. Lymphocytes were predominant in the IM subtypes, while LAR and MSL were more frequently observed in adipose tissue and vessels. Tumor spots varied in size and number depending on the subtype, with larger spots occurring in the BL and IM subtypes and smaller spots in the LAR, M, and MSL subtypes.
Deconvolution analysis showed that both tumor and stromal compartments drive TNBC subtypes. While the IM and MSL subtypes were the dominant subtypes, the LAR, M, and BL subtypes were tumor-dominant.
The tumors exhibited subtype-specific biological features, such as epithelial-mesenchymal transition (EMT) signaling in M, deoxyribonucleic acid (DNA) proliferation and repair in BL, and other metabolic pathways in LAR. Stromal compartments varied, with MSL stroma exhibiting angiogenesis and tumor-associated fibroblast activity, whereas IM stroma was enriched in immune signals.
The analysis of clinical results showed that M subtype tumors with MSL stroma have better distant recurrence-free survival. Larger tumor spots have been associated with proliferation and immune signaling, although smaller spots have been correlated with metabolism and hormonal pathways.
TLSs have been enriched in immune cells and have been associated with better patient outcomes. The 30-gene TLS signature accurately predicted TLS regions and correlated with favorable outcomes, including higher pathological complete response rates in TNBC treated with immunotherapy.
Unsupervised clustering revealed 418 molecular clusters grouped into 14 megaclusters (MCs), differing in immune activation, angiogenesis, and immune evasion. Some MCs, such as MC 9, were associated with improved outcomes, while others, such as MC 14, suggested immune suppression.
Nine distinct spatial architectures (SAs) have been identified, and some, such as SA 4, are associated with immune activation and favorable outcomes. SA analysis provided insight into therapeutic blind spots, suggesting potential targets such as poly(adenosine diphosphate) [ADP]-ribose) polymerase inhibitors (PARP), anti-cell differentiation antigen 37 (CD73) and antibody-drug conjugates for human epidermal growth factor receptor 3 (HER3) and trophoblast cell surface antigen 2 (TROP2).
Conclusions
TNBC is characterized by complex molecular and cellular heterogeneity. The current study demonstrates how ST can reveal clinically relevant tumor features, immune response, and therapeutic targets that may not be obvious in traditional classifications.
Magazine number:
- Wang, X., Venet, D., Lifrange, F., (2024) Spatial transcriptomics reveals significant heterogeneity in triple-negative breast cancer, with potential clinical implications. (10232). doi:10.1038/s41467-024-54145-w