Blog
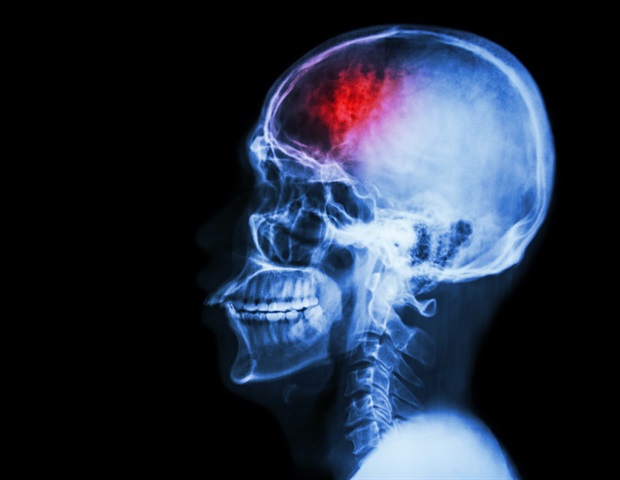
Disrupted brainstem-hippocampal connectivity identified as a biomarker of delirium
Context and goals
Delirium, commonly observed in critically ill patients following intracerebral hemorrhage (ICH), is an acute neuropsychiatric disorder characterized by disturbances in attention, consciousness, and cognition. The underlying mechanisms of the brain network remain poorly understood. The aim of this study was to investigate the functional connectivity (FC) of the ascending reticular activating system (ARAS) in delirious patients with basal ganglia ICH and to identify potential biomarkers to predict the onset of delirium.
Methods
This cross-sectional study used brain networkomics techniques to investigate FC within the ARAS in ICH patients with and without delirium. A two-sample t-test compared differences in ARAS connectivity between delirium and non-delirium groups, identifying abnormal brain regions and corresponding FC values. Receiver operating characteristic curve analysis was then performed to evaluate the predictive value of FC for the occurrence of delirium.
Results
In patients with ICH with delirium, significant FC abnormalities were observed between the ARAS nuclei of the brainstem and the left parahippocampal gyrus. FC strength between these regions was a reliable predictor of delirium, with an area under the curve of 0.893, indicating high prediction accuracy.
Conclusions
Disruption of FC between the brainstem ARAS nuclei and the left parahippocampal gyrus may underlie the pathogenesis of delirium. Appropriate FC force can serve as effective biomarker to predict the onset of delirium. Restoring normal connectivity between these regions may represent a strategy for early reversal of delirium and is a key focus for future research.
Source:
Magazine number:
Zhang, J., (2025). Disrupted brainstem connectivity of the ascending reticular system activating the left parahippocampal gyrus may reveal mechanisms of delirium after basal ganglia intracerebral hemorrhage. . doi.org/10.14218/nsss.2025.00030