Blog
Blocking GAPDH aggregation protects brain cells and opens a new path for impact therapy
Last study published in the journal He informed that inhibiting aggregation (Gapdh) could be a therapeutic goal for acute ischemic stroke (AIS).
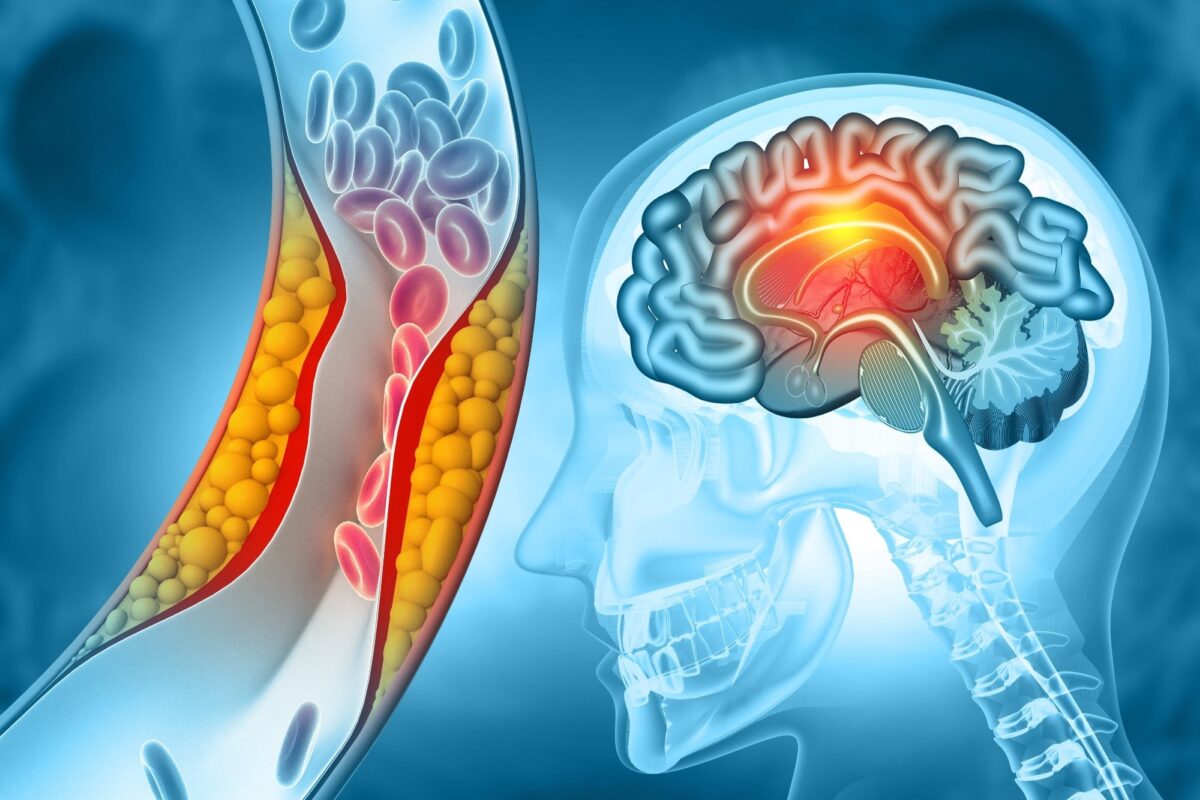
The stroke is the second main cause of death. The recombinant tissue plasminogen activator is one of the most effective AIS treatment methods, but it has limited acceptability and narrow therapeutic window (within 4.5 hours). Other drugs are symptomatic treatment and have short therapeutic windows. Therefore, new therapeutic approaches are needed to examine alternative therapies.
Evidence suggests that damage to ischemia-reperfusion plays a role in AIS pathogenesis. The brain undergoes solid nitrowose/oxidative stress during reperfusion of ischemia, which causes neuronal death. Understanding stress caused damage can illuminate the mechanisms underlying and help identify potential AIS treatment.
It is a multifunctional protein that shows various functions, including DNA repair, kinase regulation, heme metabolism and regulation of necrosis and apoptosis. With oxidative/nitose stress, nuclear translocation occurs with low to moderate stress (causing apoptosis), while aggregation occurs with severe stress (causing necrosis).
Examination and results
In this study, scientists assessed whether the aggregation caused by ischemic reperte is involved in AIS pathogenesis. First of all, the mouse model AIS was created by transient medium obstruction of the medium brain artery (MCAO). Animals were under ischemia for 30 minutes and reperfusion for different duration. The brain heart attack was visible 24 hours after the reperto, with the volume of the infarction increased over time. The aggregates were detected in stripes (ischemal core) 12 hours after the repefs, preceding a heart attack.
The team generated conditional transgenic mice with GapdH-C152A expression specific to neurons in order to check whether neurons damage can be prevented by inhibiting aggregation. To this end, they used the human construct Gapdh-C152a (which reduces aggregation in a dominant-negative manner) and doxicins to temporarily control its expression.
Gapdh-C152a was expressed in the absence of DOX, but not in its presence. In addition, transgenic and non -transgenic mice were treated with DOX or carrier for 14 days before MCAO. Physiological parameters (blood pressure, blood gases, brain blood flow) remained unchanged.
The volume of the infarction was the same at all non -utransgenic mice, regardless of DOX treatment. On the other hand, transgenic DOX mice had much smaller volume of infarction in both bark and striator than the counterparts treated DOX. In addition, the neurological result, a one-sided paralysis indicator, has been significantly improved in DOX absent transgenic mice, which suggests that GapdH-C152 expression has improved brain damage.
Scientists have previously informed that the aggregates induced mitochondria dysfunction and in vitro cell death. As such, the dysfunction of mitochondria was assessed on the basis of release of cellular death mediators: the factor induceing apoptosis (AIF) and cytochrome C (cytochrom), which enter the nucleus and cytosol accordingly. Both AIF nuclear levels and cytosol levels of Cyt C were much lower in transgenic mice absent DOX than in DOX transgenic mice.
In addition, the team assessed whether brain damage can be prevented by pharmacological inhibition of aggregation. For this purpose, peptides of various types and the number of amino acids were designed and tested in terms of their inhibitory potential. The SCT (Seryn-Treonine) tripeptide (GAI-17, IC50 = 1.18 μm) was identified as the strongest inhibitor, without the undesirable effect of cell life or enzymatic activity. Its therapeutic effects were then evaluated in the MCAO model.
Mice was injected with an intra-branch (ICV) with 30 nmol or 60 Nmol GAI-17 1 hour before, immediately after and 12 hours after the reperfusion. Initial processing of the GAI-17 significantly reduced the volume of myocardial infarction in a dose-dependent way. High -dose treatment caused a significant decrease in the volume of myocardial infarction, especially in the bark (penumbra), but not in the striator (ischemic core). GAI-17 is clearly located in neurons after ICV administration. Treatment 60 Nmol GAI-17 did not affect physiological parameters. In addition, AIF levels and cytosol levels Cyt C were significantly reduced in the bark by 60 Nmol GAI-17.
Finally, the team tried to determine the therapeutic time window. For this purpose, the GAI-17 was given at two time points: 3 hours and 12 hours (group after 3h), 6 hours and 12 hours (group after 6h) or 9 hours and 12 hours (group after 9h) after repefs. The volume of the infarction has been significantly reduced in bark in groups after 3 hours and after 6 hours. Neurological deficits have been significantly improved by GAI-17 treatment in groups after 3 hours and after 6h. However, the group after 9h lacked protective effects, establishing a therapeutic window up to 6 hours after the repefs.
Science restrictions
The examination had key restrictions: (1) only temporary ischemia (with repefsion) were modeled, not permanent stroke; (2) The effects were only rated sharply (≤48h), not in the subacute/chronic phases; (3) Potential Non-target effects GAI-17 remain unexplored; and (4) while women showed reduced susceptibility to damage, sexual differences were not fully examined.
Conclusions
The study showed that aggregates are formed before the start of the brain infarction after ischemia-reperfusion in the mouse model AIS. Discoveries suggest aggregation as a probable causal mechanism of neuronal death in AIS.
The reduction of aggregation by genetic (C152A-Gapdh) or pharmacological (GAI-17) is approaching the relaxed mitochondria dysfunction and alleviated neurological deficits and brain damage primarily in the cortical partition.
Together, the arrangements suggest that inhibiting aggregation can be a therapeutic goal for AIS, offering an extended treatment window compared to current options.